“This post may contain affiliate links, if you click a link we may earn a commission if you purchase from that merchant.”
Many people find that dental insurance plans help them in successfully budgeting for the expense of keeping a beautiful smile.
When compared to medical insurance, dental insurance plans are simple to comprehend. The majority of policies are clear and precise on which procedures are covered and how much you would pay out of pocket.
Dental insurance is offered as part of medical insurance plans or as a separate policy.
Every beautiful smile is followed by a dental plan that aids in enhancing the oral health of those who are protected by it.
However, before you select dental insurance, you should know how a plan is offered, what it includes, and how much coverage it provides for the price.
Knowing how dental insurance works will help you find the best coverage for your family’s needs and budget, whether you’re considering braces or want to keep up with cleanings.
Everyone deserves a great smile; for this reason, dental insurance policies help to budget the cost of maintaining great teeth effectively. Understanding dental insurance policies can be quite a hassle since it’s different from medical insurance.
Most, if not all, insurance has specific and straight forward policies regarding the procedures covered and the deductible that you have to incur. Dental insurance can either be a stand-alone policy or part of your medical insurance plan.
Table of Contents
How does dental insurance work?
To begin, let’s look at how private dental insurance works. You select a package depending on the types of providers (dentists) you want to choose from and your budget.
- You can pick one of the less costly options if you already have a dentist that you want and who is part of the insurance company’s network.
- If you don’t have a dentist, you can select from a list of dentists in the network and, once again, choose a less costly package.
- Also, if your existing dentist is not in the network, you can quickly get dental insurance. But you still have to pay more to see your dentist than an in-network one.
The cost of your monthly premiums is determined by the insurance provider, your state, and the policy you buy.
The monthly premium for many people would be about $50 a month. This indicates that you will still be spending $600 on dental costs per year even though you don’t get much work done.
Overview
For private dental insurance, the system allows you to select your policy based on the dentist that you wish to visit and the amount of money that you can comfortably afford to pay.
If there is a dentist whose services you like and are part of the insurance company’s network, you have the option to choose a cheaper dental insurance plan.
If you don’t have a specific dentist, it’s still ok as you have an option to choose one from the company’s network and even have the opportunity to choose a cheaper plan.
If you have your dentist who is not in the company’s network, you still get an insurance policy. The only disadvantage is that you will end up paying more to see a dentist who is not within the insurance network.
Monthly premiums for dental insurance will depend on the plan that you choose, your current location and your preferred dental insurance company
Dental insurance waiting period:
Many dental insurance plans have six to twelve-month waiting times before any regular work can be completed.
Significant work usually has a longer wait time, which can be up to two years. Insurance firms put these time limits to ensure that they benefit from a new account and prevent people from applying for a new policy to cover upcoming procedures.
Most dental insurance covers have a waiting period that ranges from 6 months to 12 months.
For dominant dental work waiting period can be as long as two years. The waiting duration is an advantage to the insurance company as it gains more profit from a new account.
Co-insurance, co-pays, and deductibles:
A deductible is the minimum amount of money you need to pay before the insurance policy pays for anything.
For example, if the deductible is $500 and the insured person’s treatment costs $450, the insurance company will not pay anything, and the individual will be liable for the entire expense. Also, you need to pay any co-pays or amount at the time of the procedure.
When the dental deductible is met, many insurance policies will only cover a certain amount of the remaining costs. This remaining balance paid by the patients is known as coinsurance, and it usually ranges from 25% to 85% of the total bill.
An insurance deductible is an amount that you, as a client, pay before the insurance company pays for any damage.
Co-pays are a set amount that you may be required to pay before any procedure. After you’ve paid the deductible, your dental insurance company covers a certain percentage of your remaining cost.
Whatever balance remains that is to be paid by the patient is referred to as co-insurance.
How Dental Insurance Categorizes and Pays for Procedures?

Dental procedures are usually classified into three categories by insurance policies: preventive, primary, and major. Most dental programs cover 100 percent of preventive treatment, such as cleanings, X-rays, and sealants, on an annual or semiannual basis.
Gum disease care, extractions, fillings, and root canals are standard procedures, with deductibles, co-pays, and coinsurance deciding the patient’s out-of-pocket costs.
The majority of policies cover 80% of these treatments, with patients responsible for the remaining 20%. Crowns, bridges, inlays, and dentures are usually only compensated 50% of the time, with the patient bearing more out-of-pocket costs than most treatments.
Every policy is different in terms of which procedures are classified as preventive, primary, or major, so it’s crucial to know what’s covered before comparing policies.
Some policies consider root canals to be effective procedures, while others consider them minor procedures that are covered to a greater extent.
Dental Insurance Does Not Cover Cosmetic Procedures
Although most medical insurance plans have annual out-of-pocket maximums, most dental insurance policies have annual coverage limits. The annual coverage maximums are usually between $1,000 and $2,000 a year.
In general, the higher the monthly premium, the greater the annual limit. Patients must account for all remaining dental treatments in full until the yearly limit has been reached.
Many insurance providers have plans that allow you to carry forward a portion of your unused annual limit to the following year.
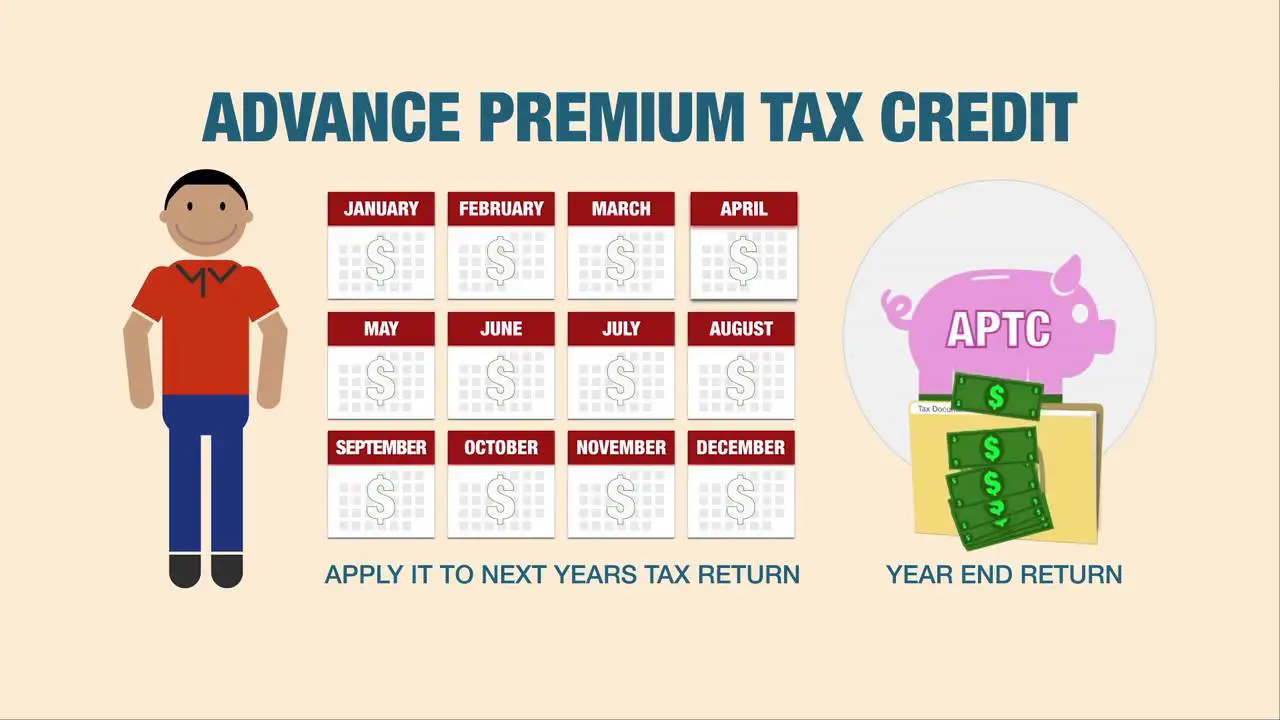
Applying Tax Credits for Dental Insurance
Suppose your medical insurance policy does not provide dental benefits. In that case, the remaining tax credit that was not used to pay for your family’s health insurance through Healthcare.gov can be applied to pediatric dental insurance premiums.
You cannot use tax incentives to purchase an extra policy if your health care policy requires dental benefits for your children.
Dental Benefits Explained | What is an Annual Maximum
Dental benefits are more critical when you understand how to use them. Understanding what dental benefits are and how they work is the first step in doing this.
To make the most of your dental coverage, discover an annual maximum on a dental plan.
Annual Maximums on Dental Plans
Depending on what you signed up for, the dental coverage will be different. Most dental plans have an annual maximum, also known as an “annual benefit maximum.”
This is the average amount that a dental benefits provider can pay for a member’s dental treatment over 12 months. That time period is called a benefit period.
A benefit period can begin at any time during the year. For now, we’ll assume your plan’s benefit period is the calendar year. That means your plan’s annual maximum refers to January through December.
Suppose your dental benefits plan’s annual maximum is $2000. In that case, your dental benefits company will pay for their portion of your dental work, depending on your plan’s coverage/coinsurance amounts, before they reach $2000.
If a treatment has cost-sharing, it will be mentioned in your plan’s details. Your dental plan’s annual maximum is reset at the beginning of each benefit cycle.
Remember that, depending on your dental plan, diagnostic and preventive services cannot be counted against your annual maximum.
The word “out-of-pocket maximum” is often confused with the annual maximum of a dental plan. The annual maximum is the most a dental benefits company can pay out in a particular plan year.
The “out-of-pocket maximum,” on the other hand, applies to the maximum amount you, the member, must pay in a single plan year.
Below we have shown in an example how the Annual Maximum of a Dental Plan works:
- Your plan has an annual maximum of $2000.
- In January, your dentist tells you you need a cavity filling. The treatment costs $200, but your dental coverage covers fillings at 80%, so you have to pay $160. (After deducting $160 from your annual maximum for the year, you have $1,840 left.)
- Then, in March, you’ll need a root canal, which will set you back $200. Root canals are covered at 80% by your dental coverage, which means you’ll be out $560. (Out of your $2000 annual limit, your dental plan has paid $320 for your dental care in this benefit period: $1680 remains.)
- In October, you’ll need a crown, which will set you back $1500. Your dental plan covers crowns at 50%, so your dental plan will cost $500. (In this case, you’ve already spent $1,070 of your $2000 annual maximum, leaving $930 available for use during your benefit period.)
- Suppose you hit the benefit period’s annual maximum, which means the insurance company has charged $2000 for your dental services. In that case, all additional services are entirely your responsibility before the next benefit period.
- Your annual maximum goes back to $2000 after your benefit period.
Is Basic Dental Insurance Worth It?
All dental insurance policies are intended to save you money on preventive dental treatments, but with a basic dental insurance plan, you’re only eligible for preventative treatment, which is 100% covered.
That means you won’t have to pay something out of pocket for essential dental services like checkups, cleanings, and bitewing x-rays.
A basic dental insurance plan costs around $25 per person, per month on average, or $300 per year for one person.
A basic dental insurance plan for a family (two adults and two children) would likely cost about $500 per year. Following are the factors that make dental insurance worthy.
- If you are getting free basic dental insurance from your employers, then it is worth it.
- Basic dental insurance can be all you need if your dental health is excellent and you purchase your insurance. Consider it a way to pay for your preventive treatment in advance, as well as an opportunity to see your dentist regularly.
- If you have dental problems, you’ll need more than just basic dental coverage. However, before you buy a regular dental insurance plan, think about the requirements. If you have dental problems that need urgent attention or would cost more than $1,000 to fix, you may want to consider a dental savings plan as an option.
Dental procedures can either be major primary or preventive. These are the three major categories.
Most dental insurance policies will cover 100% when it comes to preventive care, such as the semiannual visit to the dentist for a cleaning, sealants, and x-rays. Necessary procedures include root canal, extraction, fillings, or treating gum disease.
Necessary procedures have co-insurance, co-pays, and deductible, meaning the patient will have to pay the remaining amount. For significant systems such as dentures inlays and bridges only have a high co-payment.
This means that the patient we’ll have to chuck out a considerable amount from their pockets to cover for the expenses.
Some policies put the root canal in the major procedure category, while others see it as a necessary dental procedure.
Gum contouring, veneers, teeth shaping, and teeth whitening are not covered in the dental insurance policies since they are cosmetic procedures.